Disease Modifying & Curative Therapies
Disease Modifying Therapies
View our 2021 Living SickleSMART session: Disease Modifying Therapies in Sickle Cell Disease (by Dr. Stephen Nelson)
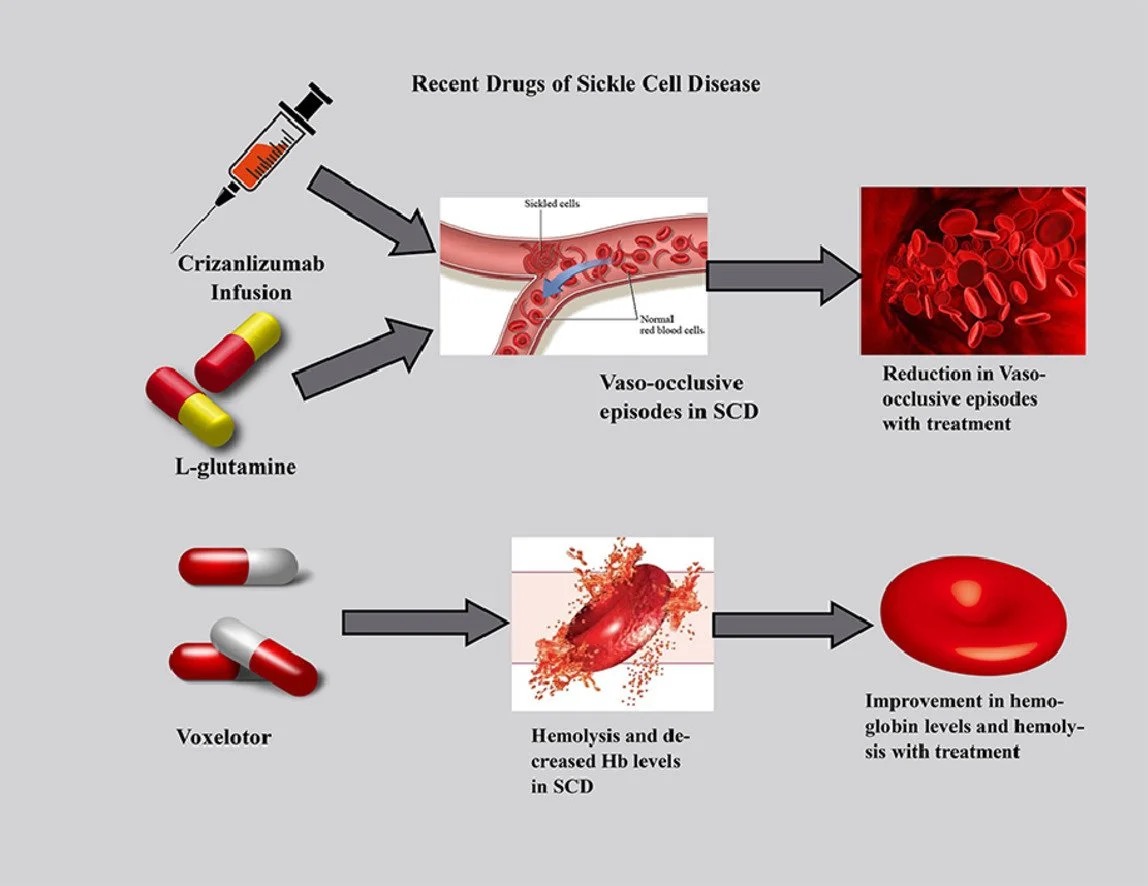
There are now more options than ever for disease modifying therapies in sickle cell and many more options are being researched or are currently in clinical trials.
Current FDA approved disease modifying drugs include: (as of 12/2021)
Hydrea/Hydroxyurea - oral capsules (daily)
Voxeletor/Oxybryta - oral tablets (daily)
Crizulizamab/Voxeletor - infusion (monthly for 12 mo)
L-Glutamine/Endari - oral powder (must be mixed w/water or juice)
NOTE: Benefits and risks exist for ALL medications. Please consult your physician to discuss your options and help determine which treatment option(s) may be right for you.
Blood Transfusions
THE SICKLE CELL COMMUNITY NEEDS YOUR HELP!
Blood transfusions are a critical component of treating sickle cell disease. For individuals living with this hemoglobin disorder, blood transfusions are used to provide normal (non-sickled) red blood cells to the patient's body, especially when facing life threatening complications such as acute chest syndrome (ACS), stroke, or other serious complications.
For many, monthly blood transfusions are needed to prevent strokes. Red blood cell transfusions help lessen anemia and reduce the blood's viscosity, allowing the patient’s blood to flow more freely and ease disease symptoms and prevent/reduce certain complications.
5 Steps to Safer Blood Transfusions If You Have SCD
Learn more at www.cdc.gov/transfusions
Share your transfusion history with your healthcare provider including:
The number of lifetime transfusions and
Any previous reactions to blood transfusions
Know your blood type and antigen profile. Ask your provider for an extended red cell antigen profile, a test that determines the special proteins on the surface of each red blood cell. Share the results with your healthcare providers before your blood transfusion.
Request blood matching. Once you and your Provider know your blood type and antigens, you can be better matched to donor blood and avoid blood that commonly causes transfusion reactions in people with SCD: C/c, E/e, and K red cell antigens.
Track your iron levels. If you/your child has received more than 10 transfusions over your lifetime, you may be at risk for iron overload. Ask your doctor for a ferritin blood test which measures the amount of iron in your blood. If your liver ferritin levels are high, your Provider may also run a Liver MRI that measures iron levels in your heart.
Talk to your Provider about YOUR transfusion options. If you need regular transfusions, ask your provider about automated red cell exchange, a transfusion process that removes and replaces sickled cells with healthy blood.
2020 ASH SCD Guidelines: Transfusion Support
Gene Therapy
Gene therapy involves altering the genetic coding inside your body's cells in an effort to treat or stop disease. Genes contain your DNA — the code that controls much of your body's form and function, from making you grow taller to regulating your body systems.
All babies in the womb and newborns have a certain version of hemoglobin called fetal hemoglobin. Even babies with sickle cell disease make normal red blood cells because fetal hemoglobin doesn't sickle. But shortly after birth, the body stops making fetal hemoglobin and starts making adult (A) hemoglobin. The reason this is critical for sickle-cell patients is that the gene mutation is what causes the body to make an adult hemoglobin variant, sickle (S) hemoglobin. Gene therapy in sickle cell works by flipping the body’s switch back to fetal hemoglobin, simultaneously increasing fetal hemoglobin, which does not sickle, and directly reducing sickling (S) hemoglobin.
To perform gene therapy, a patient’s blood stem cells are collected and exposed to a vector containing instructions to knock down BCL11A (the gene mutation that causes SCD). The patient then receives chemotherapy in a process called conditioning, likened to plowing a field to make room for new seeds. Finally, the gene-modified cells are given back via intravenous infusion.
Gene therapy (or gene editing) does not require a donor and is currently in various stages of clinical trials.
Bone Marrow Transplant
Bone marrow transplant is currently the only FDA approved cure for patients with sickle cell disease and has been used in SCD for over two decades.
A blood or marrow transplant (BMT) replaces unhealthy blood-forming cells with healthy ones. Blood-forming cells (blood stem cells) are immature cells that grow into red blood cells, white blood cells and platelets. They’re found in the soft tissue inside your bones, called bone marrow. When they’re mature, they leave the marrow and enter the bloodstream.
In order to replace the abnormal stem cells residing in bone marrow with healthy cells, there must be an eligible donor, typically a brother, sister, or parent (haploidentical transplant), however, on rare occasions an un-related match may be the only option. BMT does not involve a surgical procedure. It is performed intravenously and is just like getting blood or medicine through an IV.
In order to receive a BMT the doctor will have to find out both your human leukocyte antigen (HLA) type as well as any potential donors’ type.
Learn more about the role of Bone Marrow Transplant in curing SCD
View our Living SickleSMART discussion with Be The Match
Be The Match offers FREE HLA typing to individuals living with SCD!
Free HLA Typing
What is HLA Typing?
Human Leukocyte Antigen (HLA) is a protein found on most of the cells in your body. Doctors look for a donor or umbilical cord blood that closely matches your specific HLA in order to reduce life-threatening complications that can come with this procedure.
DID YOU KNOW? Be The Match offers FREE HLA typing to individuals living with sickle cell disease!
Learn more here.
Sickle Cell Warrior Package
Are you an individual living sickle cell disease? Are you the caregiver of a child with sickle cell disease? The new Sickle Cell Connect Program from Be The Match, connects individuals living with sickle cell disease to resources and treatment options.
Order your sickle cell warrior package from Be The Match and someone from their team will reach out to you.
Sickle Cell Patient Navigators
Patient Support Center has 3 navigators dedicated to working with sickle cell warriors and caregivers. They are able to help you learn more about transplant, connect you to resources, and provide emotional support.
Ready to talk now?
CALL OR TEXT: 1 (888) 999-6743
EMAIL: patientinfo@nmdp.org
Blood Donor Diversity
View our 2021 SickleSMART session on “Diversifying the Blood Donor Pool”
If something is FOR US, it must be WITH US
WE ARE THE US WE’VE BEEN WAITING FOR!
Since nearly the beginning, there has been a large gap between the number of individuals needing blood or bone marrow and the number of folks donating it. This gap is even wider when we are talking about people of African descent donating or having access to these life-saving donated products. In 2020, shortly after the start of the pandemic, this disparity was glaringly obvious as the shortage of blood donors created a disturbing ethical debate. Which patients get blood and which patients do not! Thankfully, the Red Cross, Be The Match, and others have stepped up to ensure that blood and marrow remains readily available to marginalized communities and chronically ill patients! To do this, they also had to make donor diversity a top priority.
So why do Black donors matter? Every ethnic group has genetic
similarities that increase compatibility markers and when medical complications such as acute chest syndrome, stroke, or transplant require a lifesaving cellular therapy, the best matches are found in similar ethnic and genetic backgrounds.
How can blood banks and the marrow registry provide life-saving therapies (such as blood transfusions and BMT) to Black communities if the safest matches come from similar ethnic groups, but many in these communities aren’t aware of the need, are unfamiliar or untrusting of the process or simply don’t donate as often as they could?!?! Simple…once we know the solution (donate!), we can do something about it!
When we think about blood transfusions for those who have had (or will have) multiple transfusions throughout their lives, it is essential for hospitals to maintain an adequate supply of closely matched blood — which is typically found in donors of the same or similar ethnicity.
Lend a hand by lending an arm!
African American blood donors play a critical role in helping to ensure that patients battling sickle cell disease receive the most compatible blood match. There aren’t enough blood donors who are African American to meet this urgent need. In 2020, the American Red Cross launched a national SCD initiative to ensure the availability of donor blood to individuals needing blood transfusions.
For more information visit www.redcross.org/sicklecell
Learn more about donating blood and donor diversity here.
Marrow Donor Diversity
If you are Black or African American, there is a less than 25% chance of finding a match on the registry!
Donor Diversity in Marrow Donations
For more than 30 years, Be The Match, operated by National Marrow Donor Program (NMDP), has been the world’s leading marrow registry organization. The work that they do saves lives, but ALL lives do not have equal access to their life saving work!
If you are Black or African American, there is a less than 25% chance of finding a match on the registry! The only way to change that is to recruit more people of African ancestry!
In an effort to increase the likelihood of finding a match, particularly for individuals living with sickle cell disease, Be The Match has launched several initiatives to increase their visibility and educate communities of color about ways they can help save lives.
Donor disparities on the registry
Learn more about how Lauren helped save the life of someone with sickle cell disease
Clinical Trials
Click here to learn more about clinical trials.
Clinical trials are medical studies that help find new ways to prevent, detect, or treat diseases that are safe and effective. These medical research trials provide valuable insight into patients, providers, and researchers. Clinical trials are necessary in the advancement of medical science. Click here to learn more about clinical trials.