Sickle Cell Disease & Trait
Sickle Cell Disease (SCD)
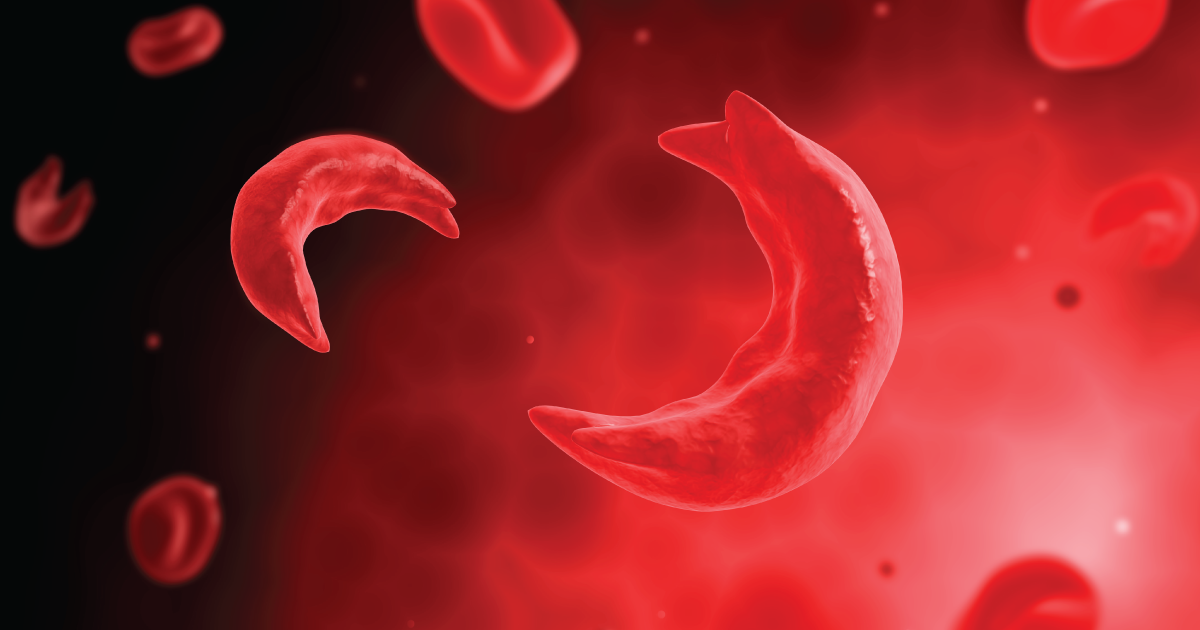
Sickle Cell Disease is a group of inherited red blood cell disorders. Healthy red blood cells are round, and they move through small blood vessels to carry oxygen to all parts of the body. In someone who has SCD, the red blood cells become hard and sticky and look like a banana, however, the disease gets its name from the affected cells looking like a C-shaped farm tool called a “sickle”. The sickle cells die early, which causes a constant shortage of red blood cells. Also, when they travel through small blood vessels, they get stuck and clog the blood flow. This can cause many very serious problems such as infection, acute chest syndrome and stroke.
In addition to other life-threatening complications, sickle cell disease is also known to cause severe and debilitating acute pain episodes that can last from days to weeks and often results in increased hospital admissions. Chronic pain from sickle cell disease can last for several years and is often mis-treated by medical professionals.
Types of Sickle Cell Disease
There are several different types of sickle cell disease; the most common types, found during newborn screening, are sickle cell anemia (SS Disease), sickle hemoglobin C (SC Disease), and sickle-cell beta thalassemia (Sß+ or Sß0 disease).
Other more rare variations of sickle cell disease include sickle hemoglobin D (SD Disease), sickle hemoglobin E (SE Disease) and sickle hemoglobin O (SO Disease). People who have these forms of SCD inherit one sickle cell gene (“S”) and one gene from an abnormal type of hemoglobin (“D”, “E”, or “O”). The severity of these rarer types of SCD varies.2
Sickle Cell Trait (SCT)
Individuals with sickle cell disease and sickle cell trait have the highest risk for having a child with sickle cell disease!
Sickle cell trait (HbAS) occurs when an individual inherits one sickle cell gene (“S”) from one parent and one normal gene (“A”) from the other parent. People with SCT do not typically have any of the signs of the disease and live a “normal” life, however, they are at the highest risk for having a child with sickle cell disease. They can also pass the trait on to their children who may then go on to have a child with sickle cell disease.
There are several kidney-related health concerns known to be associated with SCT. It may be important to ask your healthcare team for an eGFR test in order to accurately measure your kidney function. Known complications include:
Renal Medullary Carcinoma (a rare and aggressive cancer)
There may potentially be other uncommon health complications related to SCT, however, much more research and advocacy is needed. Please speak with your healthcare provider if you have any health concerns related to SCT.
Other SCT related education, fact sheets, and resources include:
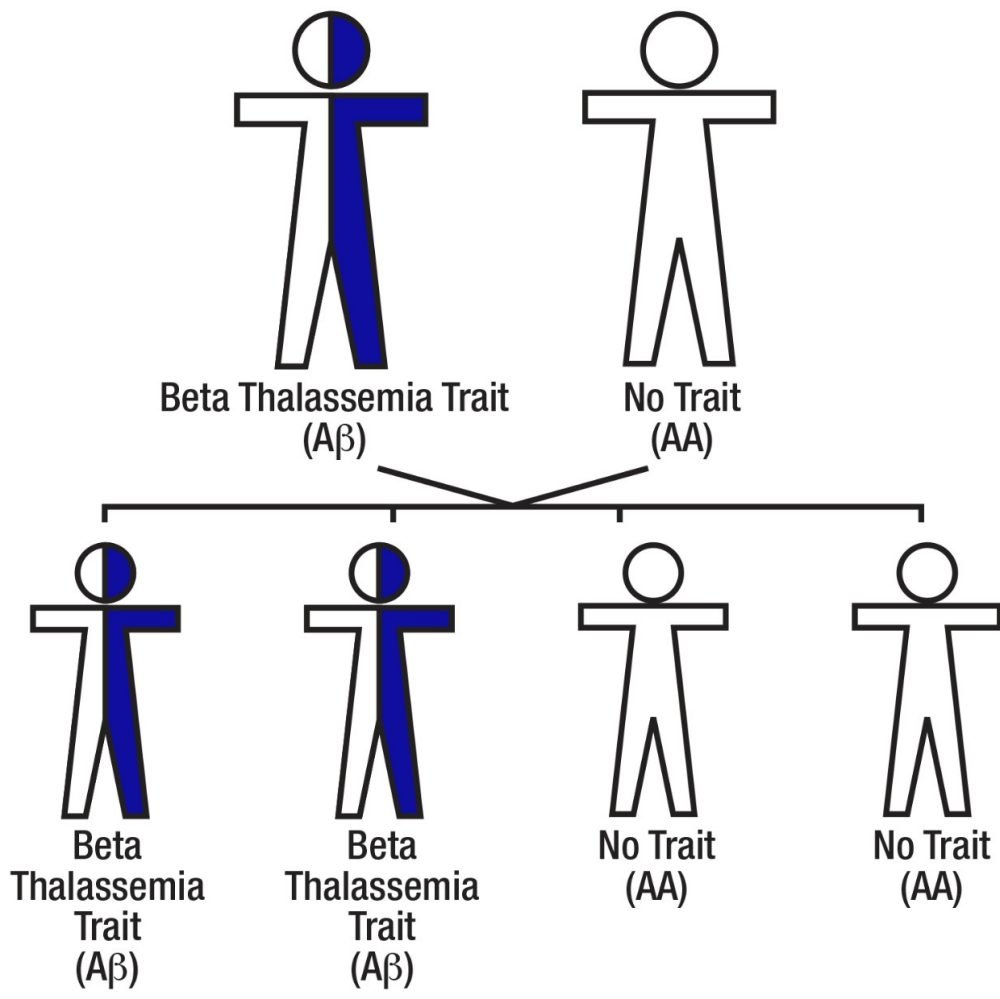
Beta Thalassemia Trait
What is beta thalassemia trait?
Beta thalassemia affects the hemoglobin in the red blood cells.
All red blood cells contain hemoglobin, which carries oxygen from the lungs to all parts of the body. People with beta thalassemia do not make enough hemoglobin.
People with beta thalassemia trait have both normal hemoglobin A and the abnormal beta thalassemia (β) hemoglobin in their red blood cells.
Beta thalassemia is common in people of African, Mediterranean, Asian and Middle Eastern descent.
Why is it important to know if I have beta thalassemia trait?
Beta thalassemia trait is inherited from one’s parents, like hair or eye color. Normally, beta thalassemia trait does not cause any health problems. Beta thalassemia trait is also known as beta thalassemia minor. If one parent has beta thalassemia trait and the other parent has normal hemoglobin A, there is a 50 percent (1 in 2) chance with each pregnancy of having a child with beta thalassemia trait. These are the possible outcomes with each pregnancy.
50 percent (1 in 2) chance of having a child with beta thalassemia trait
50 percent (1 in 2) chance of having a child without trait
Parents who have beta thalassemia trait can have a child with beta thalassemia disease or sickle cell disease (Sβ+ Thalassemia or Sβ0 thalassemia disease). This is why it is important to understand how beta thalassemia trait is passed on, and how it can affect the health of your children and grandchildren.
Sickle beta (Sβ) thalassemia disease
Sickle beta thalassemia disease is a type of sickle cell disease. If one parent has beta thalassemia trait and one parent has sickle cell trait, there is a 25 percent (1 in 4) chance with each pregnancy of having a child with sickle cell disease.
Depending on the amount of hemoglobin produced, this type of sickle cell disease is called:
Sickle beta plus (Sβ+) thalassemia
Sickle beta zero (Sβ0) thalassemia disease.
A person with sickle cell disease has red blood cells that can become “sickle or banana” shaped.
Under certain conditions, these cells can block circulation. This can cause cell damage and pain. Sickle cell disease is a lifelong illness that can result in serious health problems and require medical attention.
How is sickle beta thalassemia disease inherited?
People inherit beta thalassemia from their parents. If one parent has beta thalassemia trait and the other parent has sickle cell trait, there is a 25 percent (1 in 4) chance with each pregnancy of having a child with sickle cell (Sβ) disease. Sickle cell disease is a lifelong illness that can result in serious health problems. These are the possible outcomes with each pregnancy.
25 percent (1 in 4) chance of having a child with beta thalassemia trait
25 percent (1 in 4) chance of having a child with sickle cell trait
25 percent (1 in 4) chance of having a child with Sickle beta thalassemia disease (sickle cell disease)
25 percent (1 in 4) chance of having a child without trait or disease
This section created with information and data from St. Jude Children’s Research Hospital.
Testing & Confirmation
In the United States, SCD is most commonly found at birth during routine newborn screenings (NBS) performed at your child’s birthing hospital. These tests are done using a blood spot (or heel stick) test and then sent to the Minnesota Newborn Screening Program at the MN Department of Health to be screened for more than 50 inherited and congenital disorders. Results of blood spot screening are mailed to the birth facility or sent to the newborn’s primary health care provider if further testing is necessary. Hearing and pulse oximetry screenings are also part of the newborn screening tests.
NOTE: SickleDex test is not an appropriate method for hemoglobin screening. This test cannot distinguish sickle cell trait from sickle cell disease; it also cannot detect other hemoglobinopathy variants of SCD outside of Hgb S.
When did Minnesota (and other states) add SCD to their Newborn Screening Program? Download the list of states’ SCD newborn screening dates here.
-
1960’s - Guthrie system for collection, transport of blood
1970’s - National Sickle Cell Control Act, some states begin screening
1980’s - Efficacy of penicillin prophalaxis, NIH recommends NBS
1990’s - Most states participate in some form of NBS for SCD
2000’s - All 50 U.S. states and territories participate in NBS
2010’s - Expansion into the UK and Europe, pilot studies elsewhere
2020’s - Expansion into the Caribbean and sub-Sharan Africa
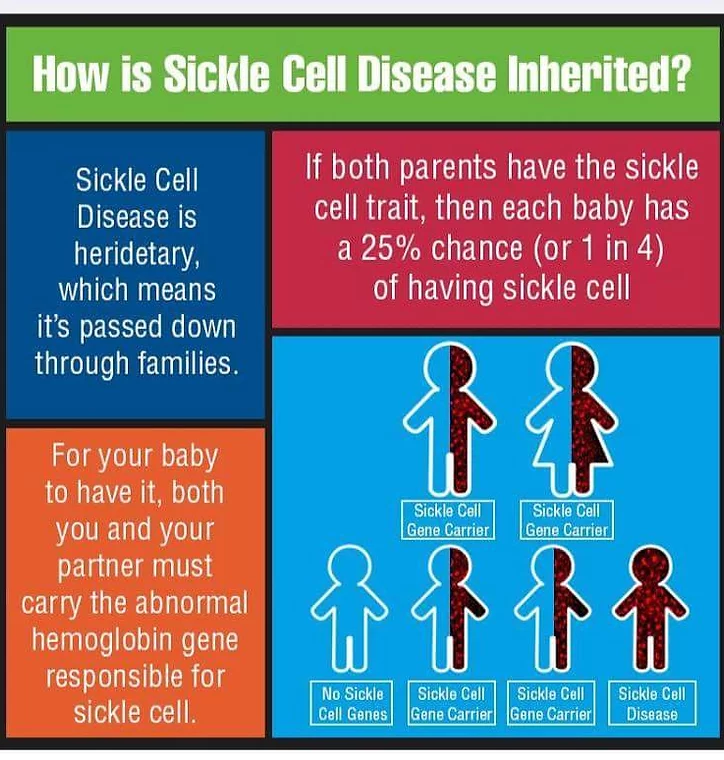
Inheritance
Genes come in pairs. You inherit 1 set from your mother and 1 set from your father.
To be born with sickle cell disease a child has fall into one of these categories:
Child must inherit a copy of the sickle cell gene from both their parents (Hbg SS/Sickle Cell Anemia)
Child must inherit a single copy of the sickle cell gene and another hemoglobin variant (Hgb C, Hgb D, Hgb E, Hgb O, etc.)
To be born with sickle cell trait a child inherits a single copy of the sickle cell gene from only one parent.
Prevalence
Sickle Cell Disease is an inherited disease and is one of the most common genetic blood disorders in the world! The exact number of people living with SCD in the U.S. is uncertain. The CDC supports sickle cell data collection projects to learn about the number of people living with SCD and to better understand how the disease impacts their health.
According to the CDC, it is estimated that:
SCD affects approximately 100,000 individuals in North American.
SCD occurs among about 1 out of every 365 Black or African-American births.
SCD occurs among about 1 out of every 16,300 Hispanic-American births.
About 1 in 13 Black or African-American babies is born with sickle cell trait (SCT).
Although sickle cell disease can be found globally, it is most commonly associated with parts of the world where malaria is or was common. This is not a coincidence! The parasite that causes malaria is interrupted by sickled cells in the body, making people who carry sickle cell trait more resistant to the disease. This is also why sickle cell trait occurs more frequently among those who are descendants of tropical and sub-tropical regions where malaria is or was common.
Sickle cell disease is believed to have originated in West Africa, where it has the highest prevalence. Much like other genetic conditions, it was a spontaneous genetic mutation to increase human survival due to malaria. It is also present to a lesser extent in India and the Mediterranean region. DNA polymorphism of the beta S gene suggests that it arose from five separate mutations: four in Africa and one in India and the Middle East. The most common of these is an allele found in Benin in West Africa. The other haplotypes are found in Senegal and Bantu, Africa, as well as in India and the Middle East.
SCD Symptoms & Complications
Pain is far from the only complication in sickle cell disease!
There are many other complications directly (and indirectly) related to this hemoglobin disorder. Regular lab tests and screenings such as transcranial doppler (TCD), pulmonary function tests (PFTs) and echocardiography (ECHO) can help to identify early warning signs of some, but not all complications.